Introduction
Prostate health is a topic of growing importance as men navigate the journey of aging. The prostate gland, though small and often overlooked, plays a significant role in a man’s well-being. Like any part of the body, it can face various health concerns that may impact the quality of life. In this comprehensive exploration, we delve into common prostate health concerns, shedding light on conditions such as Benign Prostatic Hyperplasia (BPH), Prostatitis, Prostate Cancer, and the link between Erectile Dysfunction and the prostate gland. By understanding the symptoms, risk factors, and when to seek medical attention, men can take proactive steps to safeguard their prostate health and overall vitality.
Common Prostate Health Concerns
Benign Prostatic Hyperplasia (BPH)
Often referred to as “enlarged prostate,” benign prostatic hyperplasia (BPH) is the non-cancerous growth of the prostate gland, typically occurring after age 50. As men age, it can significantly increase in size, although it is unrelated to cancer.
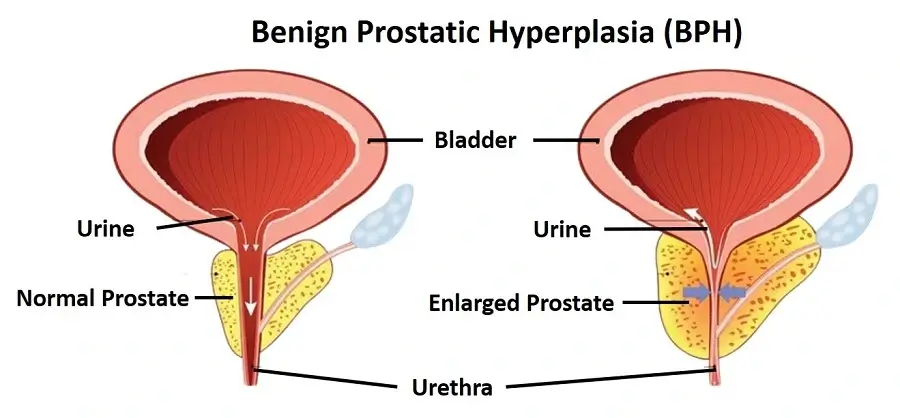
BPH constitutes a common aspect of the aging process. About half of cases show no symptoms; however, it can lead to urination difficulties as the enlarged prostate constricts the urethra, necessitating more effort from the bladder muscles. Additionally, BPH can be associated with factors such as prostatitis, a sedentary lifestyle, obesity, high blood pressure, diabetes, and a diet high in sugar, red meat, and refined grains.
BHP is primarily characterized by a set of symptoms collectively known as LUTS (lower urinary tract symptoms).
Some common symptoms associated with BHP include the following:
- Frequent urination, especially at night (nocturia)
- Difficulty starting or stopping urination
- Weak and interrupted urine stream
- sensation of incomplete bladder emptying
- Urinary urgency and dribbling.
Over time, as these symptoms progress, the obstructed prostate can lead to a condition known as acute urinary retention. In this critical situation, the bladder becomes unable to expel urine, representing a painful medical emergency due to its potential for kidney damage. Furthermore, BPH can elevate prostate-specific antigen (PSA) levels beyond the normal range.
Prostatitis – Prostate Health
Inflammation of the prostate gland characterizes prostatitis. It encompasses two main types: acute prostatitis and chronic prostatitis. Acute prostatitis arises from bacterial infection, leading to sudden pain during urination, fever, and chills.
On the other hand, chronic prostatitis, also referred to as chronic pelvic pain syndrome, often lacks a clear cause. This condition entails pelvic discomfort, painful urination, a frequent urge to urinate, and unclear origins, potentially stemming from chronic inflammation or infection. Moreover, it may involve the immune system mistakenly attacking the prostate or undetected infections. Symptoms can be triggered by certain foods, stress, depression, chronic pain, trauma to the genital area, or repeated biopsies.
Some common symptoms associated with prostatitis include the following:
- Pain or discomfort in the pelvic area.
- Frequent and urgent need to urinate.
- Pain or burning during urination.
- Blood in the urine.
- Painful ejaculation.
- Flu-like symptoms, such as fever and chills (in cases of acute bacterial prostatitis).
Some individuals may also experience a sense of rectal fullness, and blood may be present in the semen. Certain types of prostatitis can lead to spasms in the pelvic floor muscles. Although not visibly apparent to the patient, prostatitis can elevate blood levels of prostate-specific antigen (PSA).
Unlike other prostate problems, prostatitis affects younger and older men equally. However, it’s generally more common in men aged over 50. Men experiencing depression, anxiety, and stress might find prostatitis symptoms more challenging to cope with. Whereas, those with other chronic pain conditions could be more prone to it. It’s important to note that prostatitis is not contagious.
Prostate Cancer
Uncontrolled cell growth in the body initiates cancer and prostate cancer specifically originates in the prostate gland. When malignant cell growth remains confined to the prostate, it’s termed localized prostate cancer.
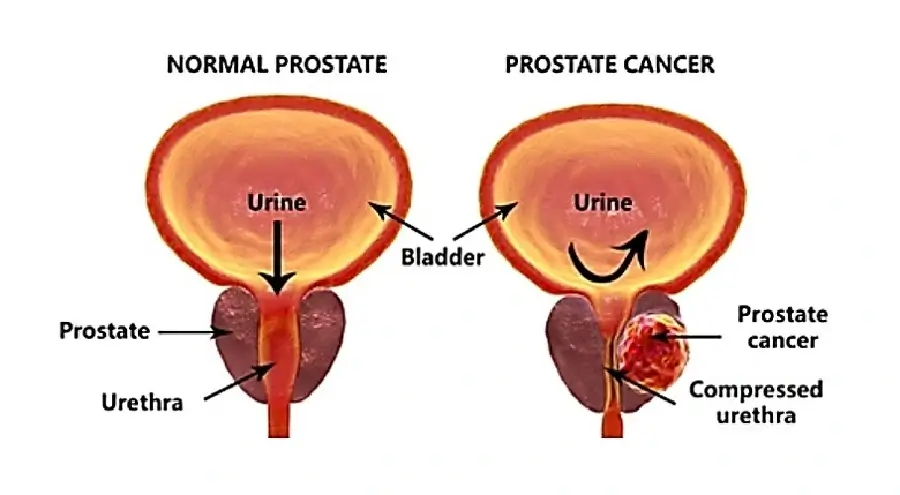
Furthermore, prostate cancer features the proliferation of malignant cells within the prostate gland. During its early stages, it may not manifest noticeable symptoms, but as it progresses, it can result in urinary issues, bone pain, and other complications. While this remains the case, the exact cause of prostate cancer remains unknown. Nonetheless, it is influenced by factors such as genetic defects, aging, family history, race (with higher rates among African Americans), diets rich in red meat and saturated fats, obesity, and infrequent ejaculation, as suggested by some studies.
In 2022, the American Cancer Society estimates that 268,490 men will receive a prostate cancer diagnosis, leading to 34,500 deaths, positioning it as the second leading cause of cancer-related deaths among American men. Despite these alarming statistics, prostate cancer often presents as low-grade and confined to the prostate, resulting in a 98% 10-year survival rate and a 96% 15-year survival rate.
Typically, low-grade cancers do not significantly impact the quality of life or lead to early mortality. However, the primary challenge lies in detecting more aggressive forms of prostate cancer at an early stage, with African Americans facing a higher risk, particularly of aggressive types, compared to other demographic groups in the US.
Early-stage prostate cancer may not cause noticeable symptoms.
Advanced prostate cancer symptoms can include:
- Difficulty urinating or a weak urine flow.
- Blood in the urine or semen.
- Erectile dysfunction.
- Pain or discomfort in the lower back, hips, or pelvis.
- Bone pain may indicate cancer that has spread to the bones.
Doctors often diagnose prostate cancer by conducting blood tests that reveal elevated PSA levels and then performing a biopsy. Moreover, many cases of prostate cancer don’t show symptoms, especially those categorized as low-risk and non-aggressive. When symptoms do appear, they typically include difficulties with urination or discomfort in the bones or back, which may suggest potential cancer spread.
Erectile Dysfunction and Prostate Health
Prostate gland issues can be linked to erectile dysfunction (ED), particularly when they affect the nerves, blood vessels, or muscles in the pelvic region. For instance, prostate problems like prostate cancer treatment or an enlarged prostate can impact erectile function, potentially causing nerve damage, reduced blood flow, or changes in pelvic muscle function.
Surgical procedures for prostate cancer, on the other hand, may damage erection-triggering nerves, while an enlarged prostate can put pressure on arteries supplying blood to the penis. However, it’s important to note that not all prostate problems lead to ED, and conversely, not all cases of ED are prostate-related. Various treatment options are available, including medications and lifestyle changes, but consulting with a healthcare provider is crucial for a personalized approach to address both the physical and emotional aspects of ED.
When should you seek medical attention for your symptoms?
If you’re experiencing lower urinary tract symptoms (LUTS) such as a weak urine stream, frequent urination, difficulty fully emptying your bladder, pain during or after ejaculation, blood in semen, or discomfort in areas like the base of the penis, perineum, lower back, or rectum, it’s important to consult a doctor. When dealing with an enlarged prostate (BPH), consider how these symptoms affect your daily life when deciding on treatment.
Factors like work, travel, and overall quality of life come into play. You can assess symptom severity using the International Prostate Symptom Score (IPSS) questionnaire, which provides an overall score. If your score falls in the moderate to severe range, it’s advisable to discuss treatment options with your doctor. In cases where you’re unable to urinate, seek immediate medical care as it constitutes a medical emergency.
Conclusion
In the realm of men’s health, prostate concerns stand as prominent challenges. Benign Prostatic Hyperplasia, Prostatitis, Prostate Cancer, and the potential link to Erectile Dysfunction all underscore the importance of monitoring and addressing prostate health. While these conditions may seem daunting, the good news is that timely awareness and medical attention can make a world of difference. Regular check-ups, a balanced lifestyle, and open communication with healthcare providers can empower men to navigate these concerns with resilience and maintain a high quality of life as they age. Prioritizing prostate health is not just a choice; it’s a pathway to lasting well-being.

